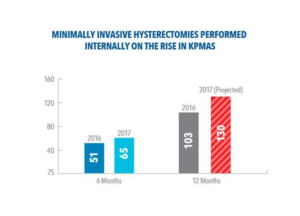
After significant work in the past few years by our Ob-Gyn physicians and Kaiser Permanente nurses and staff, MAPMG is on track to perform more than 130 minimally-invasive hysterectomies this year at our ambulatory surgery centers, a 20+ percent increase over 2016.
The expertise and training of our ASC health care teams are allowing us to internalize more and more of one of our most frequently performed surgeries in the Mid-Atlantic States, and leading to better outcomes. MAPMG physicians have also raised the overall rate of minimally invasive surgery for hysterectomy to over 90 percent in KPMAS this year, with significantly reduced post-operative complications and recovery time in our post-anesthesia clinical units and partner hospitals.
“Minimally invasive hysterectomies are beneficial to the patient because they cause less pain, it’s a shorter recovery time, there’s less scarring, less bleeding, and less injury to tissue.” said E.W. Emanuel, MD, MAPMG Associate Medical Director for Maternal Child Services and Health Education. ”We know from our own data that minimally invasive surgery in general is better for the patient and more affordable.”
Hysterectomy — a surgery to remove all or part of woman’s uterus, in response to fibroids, bleeding, or other gynecological problem — has become less and less common in recent years. About 600,000 hysterectomies are performed each year in the United States. With improved medication management and minor surgical procedures, the medical community has greater control over some of the more common causes leading to women needing hysterectomies. Medication treatments include different hormonal treatments and the use of intrauterine devices to help decrease heavy bleeding associated with menstrual cycles or fibroids. Minor surgical procedures include hysteroscopy, dilation and curettage, endometrial ablation, and uterine artery embolization – are all performed in Kaiser Permanente’s Ambulatory Surgery Centers.
When these conservative measures fail, a hysterectomy is needed. Traditionally, hysterectomies have been performed by opening up the abdomen to remove the uterus. Abdominal surgeries continue to account for about one-half to three-quarters of hysterectomies in the United States, depending on region and health care system. In recent years, however, newer minimally invasive gynecology surgery techniques, often referred to as MIGS, have been developed. In particular, surgeons can make small incisions to insert laparoscopic instruments to remove the uterus.
The American College of Obstetricians and Gynecologists supports minimally invasive hysterectomies when clinically appropriate. The vast majority of our patients go home on the same day — after about four hours. In the past, they would go home after two or three days. Patients can get back to work within a week, rather than 4-6 weeks.
Internalized MIGS are expected to top 130 procedures in 2017. As of June 30, MAPMG surgeons performed a total of 347 hysterectomies and 314 of those operations were performed using a minimally invasive procedure — mostly at our partner hospitals, Holy Cross and Virginia Hospital Center. But a growing number of these surgeries are performed in our ASCs, thanks to a concerted strategy by the medical group to improve quality and access to appropriate care.
“We don’t have to send any of our patients out,” said Dr. Emanuel, an Ob-Gyn physician by training. “Here in the Mid-Atlantic States, we can perform all of these minimally invasive surgeries. There’s not one that we externalize.”
Kevin Smith, MD, a Largo-based MAPMG gynecologist with a specialization in advanced endoscopy, said he was excited about our medical group’s focus on MIGS and our ability to build up that capability when he joined us in 2016. Dr. Smith says he’s humbled by the gratitude expressed by his patients after a minimally invasive procedure and the rapid recoveries that typically follow. “Sometimes, they’re surprised that such technology even exists,” he says. “They’re pleasantly surprised that we can offer a quicker recovery, giving them the ability to return to their normal lives, with less morbidity, and they’re generally home the same day. That’s often the most comfortable place for them to recover.”
According to a recent Kaiser Permanente study of hysterectomy patients of Northern California, patients needed an average of 48.5 hours of post-operative observation for abdominal hysterectomies, compared to 9.2 hours for minimally invasive hysterectomies. Both estimated blood loss and perioperative complications were also lower for the minimally invasive procedure: an average of 100 milliliters blood loss for minimally invasive hysterectomies (vs. 200 milliliters for abdominal hysterectomies), while perioperative complications were only 1.7 percent for minimally invasive hysterectomies (vs. 5.8 percent for abdominal hysterectomies).
Through internalization and the hard work of our MAPMG gynecology surgeons, anesthesiologists, and the support of our staff in the ASCs, our members are able to experience the value of minimally invasive procedures in the most appropriate venue for them — leading to improved quality, access, and patient experience.